News & Articles
Browse all content by date.
Definition of an “iatrogenic” disorder: A disorder inadvertently induced by a health caregiver because of a surgical, medical, drug or vaccine treatment or by a diagnostic procedure.
In last week’s column I wrote that iatrogenic disorders (a doctor-, drug-, vaccine-, surgery- or other medical treatment-caused disorder) were the third leading cause of death in the US. That revelation may have ruffled the feathers of some readers, particularly if they were employed in the medical professions, so I am enlarging on that statement in this week’s column.
In 2000, a commentary article was written by Dr Barbara Stanfield, MD, MPH. It was published in the Journal of the American Medical Association (JAMA, July 26, 2000—Vol 284, No. 4).
The article was titled “Is US Health Really the Best in the World? It has been posted at https://jamanetwork.com/journals/jama/article-abstract/192908?redirect=true.
In the article, Stanfield included the following statistics from her research about iatrogenic deaths.
(Note: these numbers do not include out-patient iatrogenic deaths):
• 12,000 deaths/year from unnecessary surgery in hospitals
• 7,000 deaths/year from medication errors in hospitals
• 20,000 deaths/year from other errors in hospitals
• 80,000 deaths/year from nosocomial infections in hospitals
• 106,000 deaths/year from non-error, adverse effects of medications in hospitals
Combining these five groups gives us a total of 225,000 in-patient deaths. The 225,000 number does not include out-patient deaths or disabilities. In any case, this number easily constitutes the third leading cause of death in the United States, behind heart disease and cancer (see the official list for 2015 below).
The CDC’s Mortality and Morbidity Report for 2000, said that cancer caused 710,701 US deaths in 2000 and heart disease caused 553,080. For comparison purposes, the CDC’s report said that heart disease caused 606,401 deaths in 2017 and cancer caused 594,707.
Below are the US death statistics for 2015 (apparently the last year that the CDC has published the complete list).
1 Heart Disease . . . . . . . . . 633,842
2 Cancer . . . . . . . . . . . . . . .595,930
3 Chronic lower
respiratory diseases . . . . . . 155,041
4 Unintentional injuries . . 146,571
5 Cerebrovascular
diseases . . . . . . . . . . . . . . . .140,323
6 Alzheimer’s disease . . . . 110,561
7 Diabetes mellitus . . . . . . .79,535
8 Influenza
and pneumonia . . . . . . . . . 57,062
9 Nephrosis,
nephrotic syndrome . . . . . .49,959
10 Suicide . . . . . . . . . . . . . .44,193
It is obvious that “Inpatient Iatrogenic Deaths” of 225,000 would easily come in 3rd, if the CDC would ever start collecting such data and publishing it as a separate category. Something fishy is going on, particularly in view of the fact that there have numerous requests that the CDC change its traditional data collection methods.
One also wonders - if more accurate figures were available – if combining in-patient and out-patient iatrogenic deaths together (a rational approach) would cause heart and cancer deaths to drop to # 2 and # 3.
One only has to consider tabulating psychiatric drug-induced suicides and homicides as iatrogenic; or logically regarding deaths from neuroleptic drug-induced diabetes and obesity to be classed as iatrogenic; or regarding the deaths from the aluminum-adjuvanted, vaccine-induced autoimmune diseases that cause so much morbidity and mortality as iatrogenic; or regarding a portion of the SIDS deaths at 2, 4 and 6 month of age, when infants are routinely injected with dangerous, untested-for-safety cocktails of mercury-containing, aluminum-adjuvanted and live virus-containing intramuscular vaccines as iatrogenic.
Or one could add in last year’s 50,000 opioid overdose deaths - most of which were prescribed by health caregivers but which were probably added to the “Accidental Death” category; or adding in the 50,000 heart attack deaths from Merck’s arthritis drug Vioxx (also iatrogenic deaths, but included in the “Heart Disease” category); or the premature chemotherapy drug-induced deaths that are invariably included in the “Cancer Death” category.
And the list of potential iatrogenic deaths goes on and on.
A decade after her article was published (in a December 2009 interview), Dr Stanfield re-affirmed the veracity of her earlier data by saying:
“106,000 people die (annually, in US hospitals) as a result of CORRECTLY prescribed medicines…Overuse of a drug or inappropriate use of a drug would not fall under the category of ‘correctly’ prescribed. Therefore, people who die after ‘overuse’ or ‘inappropriate use’ would be IN ADDITION TO the 106,000 (these numbers do not count out-patients killed by prescription drugs!) and would fall into another or other categories.” – (https://therefusers.com/is-us-health-really-the-best-in-the-world-barbara-starfield-md-mph/)
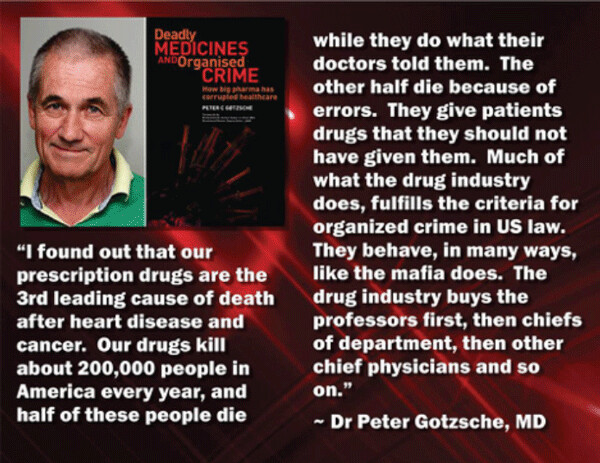
And then there is the research done by Dr Peter Goetzsche.
Dr Stanfield’s 2000 and 2009 statistics holds true for the UK and for Europe as well, according to the co-founder of The Cochrane Collaboration, Dr Peter Goetzsche. In his powerful 2013 book “Deadly Medicines and Organised Crime: How Big Pharma has Corrupted Healthcare.”
Dr Goetzsche boldly states that iatrogenic deaths should be listed as # 3 in both Europe and the US. In his 2015 companion book, Deadly Psychiatry and Organised Denial, Goetzsche makes the same points about psychiatric drug-induced deaths. Below are some quotes from his 2013 book, where he points out the many similarities between Big Pharma and the mob:
“It is scary how many similarities there are between the drug industry and the mob. The mob makes obscene amounts of money...The side effects of organized crime are killings and deaths, and the side effects are the same in this industry. The mob bribes politicians and others, and so does this industry…
“The difference is that all these people in the drug industry look upon themselves as law-abiding citizens, not as citizens who would ever rob a bank. However, when they get together as a group and manage these corporations, something seems to happen. It’s almost like when soldiers commit war crime atrocities. When you’re in a group, it’s easy to do things you otherwise wouldn’t do.” – An unnamed whistle-blowing ex-vice president for Pfizer’s global marketing department
“In contrast to the drug industry, doctors don’t harm their patients deliberately. And when they do cause harm, either accidentally, or because of the lack of knowledge, or by negligence, they harm only one patient at a time.”
“In the drug industry, bribery is routine and involves large amounts of money. Almost every type of person who can affect the interests of the industry has been bribed: doctors, hospital administrators, cabinet ministers, health inspectors, customs officers, tax assessors, drug registration officials, factory inspectors, pricing officials and political parties.”
“(As a drug rep) “it’s my job to figure out what a physician’s price is. For some it’s dinner at the finest restaurants, for others it’s enough convincing data to let them prescribe confidently and for others it’s my attention and friendship...but at the most basic level, everything is for sale and everything is an exchange.”
– Retired Drug Sales Rep Shahram Ahari “Before the approval process, the (Big Pharma-connected) sponsor sets up the clinical trial – the drug selected, and the dose and route of administration of the comparison drug (or placebo). Since the trial is designed to have one outcome, is it surprising that the comparison drug may be hobbled - given in the wrong dose, by the wrong method?
“If the trial, under these conditions, shows the drug works, the sponsors pay sub-contractors to write up the research and impart whatever spin they may; they pay ‘distinguished’ academics to add their names as ‘authors’ to give the enterprise credibility, and often publish in journals dependent on the sponsors for their existence.
“If the drug seems no good or harmful, the trial is buried and everyone is reminded of their confidentiality agreements. Unless the trial is set up in this way, the sponsor will refuse to back the trial, but even if it is set up as they wish, those same sponsors may suddenly walk away from it, leaving patients and their physicians high and dry.”
“We have a system where defendant, developers of evidence, police, judge, jury, and even court reporters are all induced to arrive at one conclusion in favour of the new drug.”
“More than 80 million prescriptions for psychiatric drugs are written in the UK every year. Not only are these drugs often entirely unnecessary and ineffective, but they can also turn patients into addicts, cause crippling side-effects – and kill.”
If any reader has any doubt about the veracity of the Stanfield and Goetzsche claims, below are a couple of other courageous researchers that have delved into the issue. In 2016, a group of Johns Hopkins medical school researchers, led by Dr Martin Makary, published supporting information in the British Medical Journal. (BMJ 2016; 353).
In the introduction of the publication, Makary and his co-authors wrote about how flawed is the CDC system of data collection and analysis:
“The annual list of the most common causes of death in the United States, compiled by the Centers for Disease Control and Prevention (CDC), informs public awareness and national research priorities each year. The list is created using death certificates filled out by physicians, funeral directors, medical examiners, and coroners.
“However, a major limitation of the death certificate is that it relies on assigning an International Classification of Disease (ICD) code to the cause of death. As a result, causes of death not associated with an ICD code (including many iatrogenic disorders), such as human and system factors, are not captured.
“…communication breakdowns, diagnostic errors, poor judgment, and inadequate skill can directly result in patient harm and death. We analyzed the scientific literature on medical error to identify its contribution to US deaths in relation to causes listed by the CDC.
Death From Medical Care Itself
“Medical error has been defined as an unintended act (either of omission or commission) or one that does not achieve its intended outcome, the failure of a planned action to be completed as intended (an error of execution), the use of a wrong plan to achieve an aim (an error of planning), or a deviation from the process of care that may or may not cause harm to the patient. Patient harm from medical error can occur at the individual or system level. The taxonomy of errors is expanding to better categorize preventable factors and events. We focus on preventable lethal events to highlight the scale of potential for improvement.”
Makary’s group published data that supports iatrogenic deaths as the # 3 cause of death.
In a 2016 open letter to the CDC, Makary’s group urged the agency to add medical errors to its annual list of common causes of death.
The letter said, in part:
“We are writing this letter to respectfully ask the Centers for Disease Control and Prevention (CDC) to change the way it collects our country’s national vital health statistics each year. The list of most common causes of death published is very important – it informs our country’s research and public health priorities each year. The current methodology used to generate the list has what we believe to be a serious limitation. As a result, the list has neglected to identify the third leading cause of death in the U.S. – medical error.”
As a partial defense of over-busy, over-booked, sometimes mentally and physically exhausted health caregivers in the US, another researcher, Dr John James, has published an article in the Journal of Patient Safety. Dr James makes similar claims urging the CDC to evaluate death statistics more logically.
The title of his 2013 article is “A New, Evidence-based Estimate of Patient Harms Associated with Hospital Care”. (Journal of Patient Safety: September 2013 - Volume 9 - Issue 3 - p 122–128)
Below are some excerpts from that article:
Using a weighted average of the 4 studies, a lower limit of 210,000 deaths per year was associated with preventable harm in hospitals…the true number of premature deaths associated with preventable harm to patients was estimated at more than 400,000 per year. Serious (but non-lethal) harm seems to be 10- to 20-fold more common than lethal harm.
Conclusions
The epidemic of patient harm in hospitals must be taken more seriously if it is to be curtailed. Fully engaging patients and their advocates during hospital care, systematically seeking the patients’ voice in identifying harms, transparent accountability for harm, and intentional correction of root causes of harm will be necessary to accomplish this goal.
“Medical care in the United States is technically complex at the individual provider level, at the system level, and at the national level. The amount of new knowledge generated each year by clinical research that applies directly to patient care can easily overwhelm the individual physician trying to optimize the care of his patients.”
“Because of increased production demands, providers may be expected to give care in suboptimal working conditions, with decreased staff, and a shortage of physicians, which leads to fatigue and burnout. It should be no surprise that preventable adverse events that harm patients are frighteningly common in this highly technical, rapidly changing, and poorly integrated industry. The picture is further complicated by a lack of transparency and limited accountability for errors that harm patients.“
“In a sense, it does not matter whether the deaths of 100,000, 200,000 or 400,000 Americans each year are associated with preventable adverse events in hospitals….one must hope that the present, evidence-based estimate of 400,000+ deaths per year will foster an outcry for overdue changes and increased vigilance in medical care to address the problem of harm to patients who come to a hospital seeking only to be healed.”
| Tweet |